Are You Measuring Patient Experience All Wrong?
// By James A. Gardner //

In a health care setting, satisfaction focuses on the gap between patients’ expectations and their experiences. Importantly, patient experience includes everything from your physical facility and clinical team to your food service and website.
And yet many health care marketers rely on narrow satisfaction measurement tools. The two most common tools — satisfaction surveys and federal HCAHPS data — while helpful to a degree, both have deficiencies that can confuse your improvement efforts.
The Net Promoter Score® (NPS) framework is built on the better idea of measuring advocacy, not just satisfaction: how many fans you have, how fanatical they are, and why they feel that way.
It asks two simple questions: On a scale of 0 (not at all likely) to 10 (extremely likely), how likely is it that you would recommend this hospital to a friend or colleague? Why do you say that?
Turning patients into fans is easier said than done, but research suggests a few especially impactful levers. Nurse and physician empathy, open lines of communication, positive clinical outcomes, and physical environment top the list.
If improved patient experience is your goal, find your “North Star” by focusing on things that matter and going beyond satisfaction to measure advocacy.
Does any hospital leader seriously question the importance of patient satisfaction? We hope not. Consumerized health care has empowered patients with choice and made exceeding their expectations a top-to-bottom priority. But what if you and your hospital were measuring patient satisfaction incorrectly? Worse, what if you were focused on improving things that didn’t really matter — and overlooking things that did?

What Exactly Is Patient Satisfaction?
Let’s first get clear on our terminology. Customer satisfaction is generally a measure of how well a product or service meets expectations. In a health care setting, satisfaction focuses on the gap between patients’ expectations and their experiences — all the interactions (including but not limited to care) that they have with your hospital, systems, clinicians, and staff.
Patient satisfaction is intentionally an all-encompassing metric. Expectations are both stated and unstated, fair and unfair, realistic and unrealistic. And well beyond care, patient experience includes everything from your physical facility and clinical team to your food service and website. If it’s seen, heard, felt, tasted, or smelled, it’s part of the patient experience.
Why Does Patient Satisfaction Matter?
Empowered patients choose where, when, and how they manage their health. As a hospital, this translates to dollars and cents: If you’re not meeting their needs and expectations, someone else will. More important, patient satisfaction has been shown to be highly correlated with quality of care, safety, and outcomes.
In a 2010 review of the relationship between patient satisfaction scores and measures of quality and safety, researchers found that patients’ overall hospital rating and willingness to recommend the hospital had “strong relationships with technical performance in all medical conditions and surgical care.”
So improve patient satisfaction and you’ll likely end up delivering better financial results and better care.
Why HCAHPS Doesn’t Solve the Problem
We can’t overlook one important measure of patient satisfaction: The Hospital Consumer Assessment of Healthcare Providers and Systems Survey (HCAHPS). Administered by the Centers for Medicare and Medicaid Services (CMS), it’s a standardized survey used to measure patients’ perspectives of care and enable head-to-head hospital comparisons.
At first blush, HCAHPS looks to be an ideal gauge of patient satisfaction. It covers multiple facets of the patient experience, is rigorously administered by CMS, and has a massive pool of respondents.
For all these reasons, HCAHPS has become the de facto public scoreboard for hospital leaders looking to show evidence of excellent care. HCAHPS is also used to help set Medicare and Medicaid reimbursement rates — so even your CFO is paying attention to it.
Scratch the surface, though, and HCAHPS is far from a perfect tool for measuring patient satisfaction.
Its questions cover only a very limited part of the overall patient experience. Nothing’s asked about wait times, for instance. Bill paying and food service, well-known pain points, are similarly overlooked, as are your hospital’s website, parking, visitor amenities, linens and furnishings, and dozens of other aspects of the experience.
So HCAHPS basically is very limited in its scope, and provides high-level data months after the fact. If your hospital is maniacally “caring to the test,” you’re missing the point and likely won’t see an increase in patient satisfaction. It’s simply not what the survey was designed to do.
New Ways of Measuring Patient Satisfaction

Brian Gresh, president of Loyal
There is growing interest in new ways of measuring patient satisfaction. Physicians are frequently reviewed and rated by patients on websites like Yelp, Healthgrades, Google, Facebook, and WebMD. There can be colorful stories here for hospital leaders, but the information tends to be very anecdotal.
There’s another problem, too. “I’d really be concerned about relying on reviews from people who may not be actual patients,“ notes Brian Gresh, president of Loyal and a veteran of the Cleveland Clinic. Loyal offers hospitals a platform for managing verified patient reviews.

Kate Madden-Jones, VP marketing and communications at Loyal
Loyal’s head of marketing, Kate Madden-Jones, a veteran of Piedmont Health, adds that many opinions on these review sites represent extreme viewpoints. “You’ll mostly hear from the happiest and the angriest people. The vast middle stays quiet,” she says.
Similar review and rating services exist for hospitals, but most of these rely on aggregate outcome and quality data, not patient satisfaction. There’s little actionable information here that would help inform hospital decision-making.

John Brownstein, chief innovation officer at Boston Children’s Hospital
Deriving sentiment and insight from social media posts is an emerging field worth watching. John Brownstein at Boston Children’s Hospital leads a team that’s shown promising results by “mining” Twitter for mentions of patient experience. There’s still much work to be done, but the promise of real-time and granular information is alluring.
A Better Way: Advocacy-Driven Metrics
Let’s step back. What if there were a metric that built on the idea of patient satisfaction — a limited idea — and extended it to the bigger idea of advocacy? Patient advocates are not only highly satisfied, but they willingly recommend and even defend your hospital to friends, colleagues, and loved ones. They’re fans (and sometimes fanatics). That’s a much higher standard than mere satisfaction.

Craig Kartchner, AVP of growth and performance marketing at HonorHealth
Craig Kartchner, HonorHealth’s AVP of growth and performance marketing, agrees. “Satisfaction isn’t enough. We often hear from customers of our hospitals who had good experiences — but who still won’t recommend us for various reasons. Aiming higher makes sense as we aspire to loyalty and advocacy,” he says.
The Net Promoter Score® (NPS) framework is built on the idea of measuring advocacy: how many fans you actually have, how fanatical they are, and why they feel that way. Done right, it asks at least one, and ideally two, deceptively simple questions:
- On a scale of 0 (not at all likely) to 10 (extremely likely), how likely is it that you would recommend this hospital to a friend or colleague?
- Why do you say that?
That’s all there is to it. Respondents are scored as promoters (9-10), passives (7-8), or detractors (0-6), and your hospital’s score is the difference between promoters and detractors. Passives don’t help or hurt since they’re considered neutral.
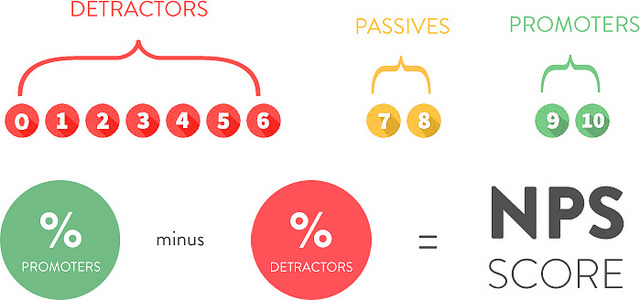
The index can range between -100 and +100. Scores higher than 0 are considered solid and scores above 50 are considered excellent. Customer experience leaders like Nordstrom, Amazon, Starbucks, Wegman’s, Netflix, and Apple all boast scores well above 50. Financial services provider USAA’s score exceeds 90, a truly exceptional performance.
Kartchner from HonorHealth likes the NPS system’s universality. “Like it or not, our system’s customers compare us to Starbucks and Apple, so we should, too,” he says. The system recently made NPS part of its larger management scoreboard and believes that the focus on advocacy will prove helpful.

Joseph Narvaez, director, data & business intelligence, office of patient & customer experience at Northwell Health
The second open-ended NPS question captures verbatim feedback. In aggregate, these comments can be analyzed for patterns that can help explain your score and competitive position. Individually, they also offer insights because of their color and specificity.
At Northwell Health, Joseph Narvaez of its office of patient & customer experience is exploring how artificial intelligence could programmatically interpret open-ended HCAHPS and NPS comments at scale. “This could supplement the limitations of our quantitative data in a really interesting way,” he notes. Like HonorHealth, Northwell also uses NPS as a key part of its patient experience measurement system.
Challenges of Turning Patients into Fans
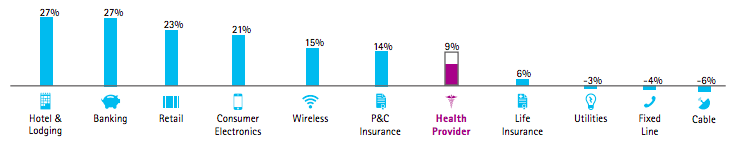
If you don’t know your hospital’s current net promoter score, prepare for a potential surprise. According to data from Accenture, health care providers score on average a lukewarm 9, slightly better than life insurers (6) but well behind hospitality and banking (both 27), retail (23), and even wireless (15).
The middling score is understandable. The very nature of health care makes the goal of patient-as-fans a challenging one. Care delivery is inherently complex. Nobody chooses to fall ill and need care. Not all patients can be healed. Affordability problems are undeniable. There’s a long list of hurdles, and real change can often seem near impossible.
Patient experience matters — a lot. If improving it is your goal, find your “North Star” by going beyond satisfaction to measure advocacy and then focusing on the things that matter most. Measurement, after all, is the first step that leads to control and eventually to improvement.
Acknowledgments: The author thanks Craig Kartchner of HonorHealth; Suzanne Hendery of Renown Health; Jared Johnson of Phoenix Children’s Hospital; Jeremy Rogers of IU Health; Chad Mallory, Brian Gresh, and Kate Madden-Jones of Loyal; Matt Gove of Piedmont Health; and Emily Kagan Trenchard and Joseph Narvaez of Northwell Health for their kind support and suggestions. No endorsement is implied.
James A. Gardner leads national market + business development efforts for MedTouch, a digital marketing agency serving hospitals and health systems nationally. James has served senior clients as a consultant with McKinsey & Company, led complex digital projects with Boston-area agencies, and built several high-performing marketing teams. He’s also been published and quoted in multiple professional publications, most recently CMSWire, CIO.com, eHealthcare Strategy & Trends, and MedTech Boston. Follow James on Twitter at @jamesagardner.