Strategies to Help Your Hospital Win at Value-Based Population Health Management
// By David Wildebrandt //
 There’s no denying it: Value-based population health management is here to stay. But how can hospitals best manage the transition from a fee-for-service approach to treating sickness to adopting one that focuses on keeping patients well in the first place? The reality is that there’s no one strategy to win this new game but rather multiple ways to make the chips fall in the most desirable way.
There’s no denying it: Value-based population health management is here to stay. But how can hospitals best manage the transition from a fee-for-service approach to treating sickness to adopting one that focuses on keeping patients well in the first place? The reality is that there’s no one strategy to win this new game but rather multiple ways to make the chips fall in the most desirable way.
Rethinking the “Old” Way of Doing Business
As a former hospital system president, I can tell you that until recently, hospitals thrived in a “sick care” role. In other words, the hospitals’ economic engines and business models have been fueled by the volume of sick patients treated. For decades, hospital success has been defined by volume metrics and top-line revenue growth. This is further evidenced by the abundance of strategies centered on grabbing market share and a maniacal focus on increasing admissions.
Accompanying these strategies has been the evolution of a leadership team whose members have been valued for being growth-minded dealmakers. Thus, when the economic foundation is turned upside down, this generation of leaders finds its skill set exposed, and what happens is the beginning of an acumen shift in health care leadership.
Moving Toward Capitation
In 2014, the American Hospital Association conducted an online survey of board chairs and C-suite executives from health systems across the country, receiving 1,078 responses from more than 400 hospitals. More than half of respondents estimated that 20 percent to 40 percent of hospital payments will be capitated over the next five years, and more than 20 percent of respondents estimated that 40 percent to 60 percent of the hospital payments will be capitated. To put that in perspective, today less than 10 percent are capitated.
These responses demonstrate that board chairs and C-suite executives are not contemplating “if” but are more focused on the “when” of value-based payment.
Most organizations still have one foot on the dock (fee for service) and one on the boat (value-based reimbursement). As the boat pulls away, they will have to go all-in or be left behind. This has forced many organizations to scramble for partners and to answer the “build, buy, or partner” question.In the aforementioned survey, 72 percent of respondents from 100- to 300-bed hospitals said they plan on partnering or experimenting with value, while 61 percent of respondents from 300-plus-bed hospitals said they also plan to do so.
The Need for a Coordinated Approach
One of the key difficulties on the value-based journey is that there is no clear linear path to success, but rather a mosaic of strategies that must be deployed simultaneously. This has overwhelmed many leadership teams as they struggled to manage competing priorities and create the needed bandwidth to succeed. The time is now to formulate a fundamentally new strategy to transition to a value-based-care delivery system. The core of this strategy should be maximizing value for patients—that is, achieving the best outcomes at the lowest cost.
 Organizations must shift from a supply-driven health care system organized around what physicians do and toward a patient-centered system organized around what patients need. The goals and measures focused on volume and profitability must be replaced with metrics centered around patient outcomes and experiences.
Organizations must shift from a supply-driven health care system organized around what physicians do and toward a patient-centered system organized around what patients need. The goals and measures focused on volume and profitability must be replaced with metrics centered around patient outcomes and experiences.
No Outcomes, No Incomes
With that said, the first role of the hospital in population health management is to take the same patient-centered culture that’s been the focus and redirect their team to a new vision. There can no longer be one foot on the dock and one on the pier. “No margin, no mission” chants must be replaced with “No outcomes, no incomes.” Hospitals have demonstrated that when they align behind a common vision, incredible things can happen. Core to this cultural transformation is the recognition of an emerging skill set and acumen. This was a resounding topic in the recent American Hospital Association survey, in which CEOs identified the primary top talent gaps in their organizations:
- Community and population health management experience
- Data analytics
- Nontraditional health partnerships (e.g., joint ventures, strategic partnerships with payers, or retailers)
- Transformational change/change management
Putting It All Together
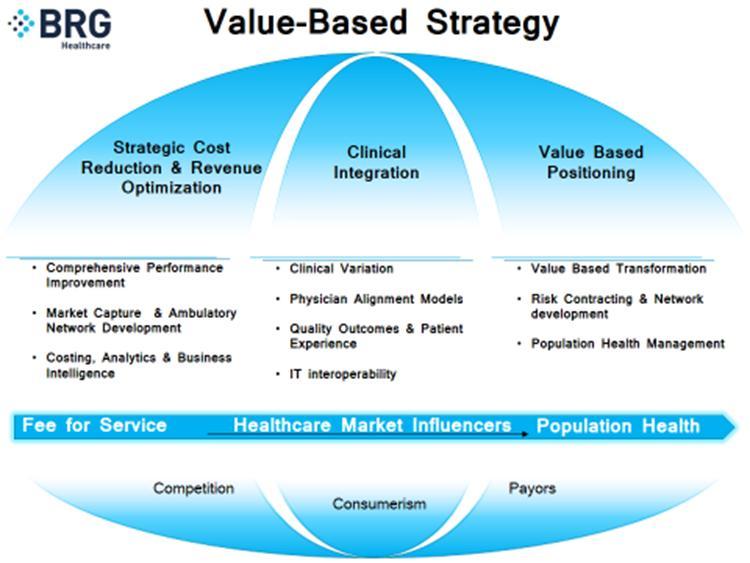
Health care leadership must first be able to create a model and an accompanying vernacular that can capture the essence of value-based transformation and assimilate all disparate pieces. The following illustration depicts a value-based strategy model and shows how organizations can create a roadmap to navigate the volume-to-value transition.
Keeping Pace in the Real World
Foundational to any market are the timing and rate of change from fee-for-service to population health. It is no longer enough to admire the problem and simply detail out the philosophy to achieve this transformation. High-performing health systems will need to continuously evaluate the health care market influencers (e.g., as competitive positioning, consumerism, and employer/payer dynamics) and adjust their strategies to keep pace with these influencers.
Exploring the Strategies
Many strategies may make sense in a volume- and value-based environment. These include:
- A focus on cost reduction and revenue optimization.
This first category must become part of how health systems operate and not an intermittent initiative. Systems must be willing to be more comprehensive and dig deeper in their cost-reduction strategies.Cost reduction and revenue optimization should focus on costs and revenues associated with workforce, human resources, supply chain, revenue cycle, clinical variation/utilization, physician practice management, and related subsidies, as well as patient throughput. A deep approach on all of these areas is still very fruitful and should be hardwired into daily operations. These should be a core competency of any organization.
- A focus on ambulatory network development and information exchange.
The next strategy is to focus on market capture and ambulatory network development. Volume is still king, and it is even more critical in organizations on the journey to risk. A tectonic shift has to occur from being hospital-centric to ambulatory-centric. The hospital can no longer exist without integration with the ambulatory setting. It must have a robust ambulatory network development strategy that is forward looking and incorporates all stakeholders. Paramount to success in a value-based world is forging new partnerships with community organizations outside the walls of the hospital. A “single source of truth” must be established around data integrity, creating unprecedented actionable information to drive performance improvement. Accurate longitudinal and integrated patient data cannot be viewed as a luxury but as a requirement to be called a health system. When armed with complete and trusted data, your leadership team will unleash a new level of performance.
- A focus on clinical integration.
The next component of a value-based strategy is obtaining buy-in from the clinical team. Today, systems must be willing to take risks, hand over the keys, and allow physicians to co-lead these strategies. Physicians will engage when they understand the root-cause issues and help craft the solution.The key to health systems thriving in a population health world is that physicians across the continuum must understand the total cost of care, and not just the cost in their area of expertise. In this environment, physicians become heat-seeking missiles looking for opportunities to improve quality and decrease costs. This is possible through a clinically integrated model where incentives are aligned and physicians share in the financial rewards.
Improving the Health of the Community
Many elements of a value-based strategy are sometimes easy to say but hard to do. In a rear-view-mirror world of top-line revenue, our true north was to grow our volume and lower our costs. There is no longer a single way to win, but instead a mosaic of strategies to enable health systems to thrive in today’s environment while leading the way for value-based transformation. The boat is pulling away from the dock, and it is no longer possible to maintain a foothold in both worlds.
The transition from a hospital-centric model to a model that improves the health of the community will take renewed vision. The outcome will be a shift in focus of the leadership talent that currently resides on the hospital team, accompanied by the sprinkling of new skill sets that will fill the gaps left behind by the fee-for-service model. Hospitals, because of their resiliency and patient-centered culture, will not end up being cost centers in the new world, but rather will lead the way.
How to Put Theory into Action for Success
While the path of every health care system toward integrating value-based care will be different, many successful groups share common elements. For instance, some health care systems that are getting it right have made value-based initiatives a part of their strategic plan and hardwired this into their timelines. By this, I mean a deliberate and measurable plan to achieve the transformation versus sprinkling in a few initiatives. Initiatives or tactics need to map back to an overarching strategy. This provides clarity to the board, medical staff, and leadership team that a value-based strategy is an imperative for thriving in the future.
Organizations on the right path also share a focus on getting the new data set deployed. In organizations I have led, any success we had was due to having optics on the right data that drove organizational outcomes. We became very efficient at responding to the data whether it was financial, quality, or patient experience data. A great example of this in the recent past was focus on improving quality. Excellent quality had no standardized definition and mostly we measured processes and not outcomes. It wasn’t until we got real-time, meaningful quality data that health systems started to move the dial.
Likewise, most health systems lack data around value-based care. We must routinely look at claims data, post-acute data, and the total cost of care data for a cohort of patients. Once you start to share this with your leadership team and physicians, the transformation is underway. That’s true, even if you simply experiment, for example by looking at your self-insured health plan data to reduce utilization and cost or directing your clinically integrated network to participate in a commercial accountable care organization. These experiments can coexist with other fee-for-service activities, and that is okay. When the economic drivers of a risk-based environment align, you will have built the acumen and infrastructure to be successful.
David Wildebrandt is a member of the Berkeley Research Group’s (BRG) Healthcare Performance Improvement practice. He brings more than 15 years of health care operations experience to this role, including having served as Senior Vice President for Baptist Health Care in Northwest Florida, and as President for Baptist Hospital Inc.