More Empathy, Fewer Spreadsheets, Better Cancer Care
How the University of Maryland Medical System leveraged journey mapping to align marketing with the patient experience.
// By Amanda Green //
 The University of Maryland Medical System (UMMS) operates 11 hospitals, more than 150 care sites, and provides greater than 25 percent of inpatient care in the state of Maryland. It’s an anchor in the Baltimore community, serving some of the state’s most needs-based patients. Baltimoreans have several choices — and great need — for cancer care. The city’s incidence of cancer is higher than the rest of Maryland and the national average.
The University of Maryland Medical System (UMMS) operates 11 hospitals, more than 150 care sites, and provides greater than 25 percent of inpatient care in the state of Maryland. It’s an anchor in the Baltimore community, serving some of the state’s most needs-based patients. Baltimoreans have several choices — and great need — for cancer care. The city’s incidence of cancer is higher than the rest of Maryland and the national average.
By late 2026, UMMS will double the footprint of the University of Maryland Greenebaum Comprehensive Cancer Center with the completion of the Roslyn and Leonard Stoler Center for Advanced Medicine, a state-of-the-art complex that will provide inpatient and outpatient services.

Jim McMahon, vice president of marketing and communications, University of Maryland Medical System
Ahead of the opening, UMMS wanted to examine the current breast cancer patient experience at the Greenebaum Comprehensive Cancer Center (UMGCCC) and how it impacts patient and referring provider choice. Jim McMahon, vice president of marketing and communications at UMMS, suggested patient journey mapping.
“The natural next question was, ‘Why is this idea coming from marketing, not patient experience or operations?’” recalls McMahon. “This is why: Marketers make a brand promise at the top that needs to be paid off at the experience level. If that doesn’t happen, we erode consumer confidence and lose patients’ trust.”
Read on to learn how a leadership team of cancer experts came together to create a shared understanding of the patient experience, and how hearing directly from patients refined their perceptions and guided the changes they made.
The state-of-the-art Roslyn and Leonard Stoler Center for Advanced Medicine is on track to open in late 2026. It will have the latest technology for evaluation and treatment, dedicated space for bone marrow transplants and cellular therapies, and modern waiting areas and rooms.

Deeper Understanding of Breast Cancer Patients
Patient journey mapping provides qualitative insights into three categories of patient experience:
- Place: How clinical sites look and feel.
- Process: The experience of receiving care at an institution.
- People: Interactions with providers and associates.

Steve Koch, managing partner, Cast & Hue
McMahon’s team partnered with Cast & Hue, a human-centered design consultancy, to lead the process.
“Health care systems have CAHPS scores, anecdotal feedback, reviews, but these can’t tell the full story,” explains Steve Koch, managing partner at Cast & Hue. “Journey mapping helps systems understand each of the defining moments in the patient experience, so they can start to understand the problems.”
After uncovering the “why,” various departments at the University of Maryland Greenebaum Comprehensive Cancer Center (UMGCCC) could strategically align efforts to address patient pain points and accentuate areas of strength.
Step 1: Socialize & Educate
Getting the right people on board early.
The process began with meetings with the broad leadership of UMGCCC.
“As we socialized patient journey mapping, we explained that this is an exercise in root cause analysis, which really resonates with health care providers,” McMahon says. “The symptom of a problem might be downstream, but the cause of it is likely upstream.”
Step 2: Stakeholder Workshop
Aligning the problem(s) to solve with the approach.
Oncologists, radiation oncologists, surgeons, nurse navigators, operations leadership at clinics, and others most deeply involved in breast cancer care attended a virtual workshop.
Through an interactive Mural session, the group shared their perceptions of the current patient experience, considered what they wanted to learn, and imagined what an ideal patient experience would look like.
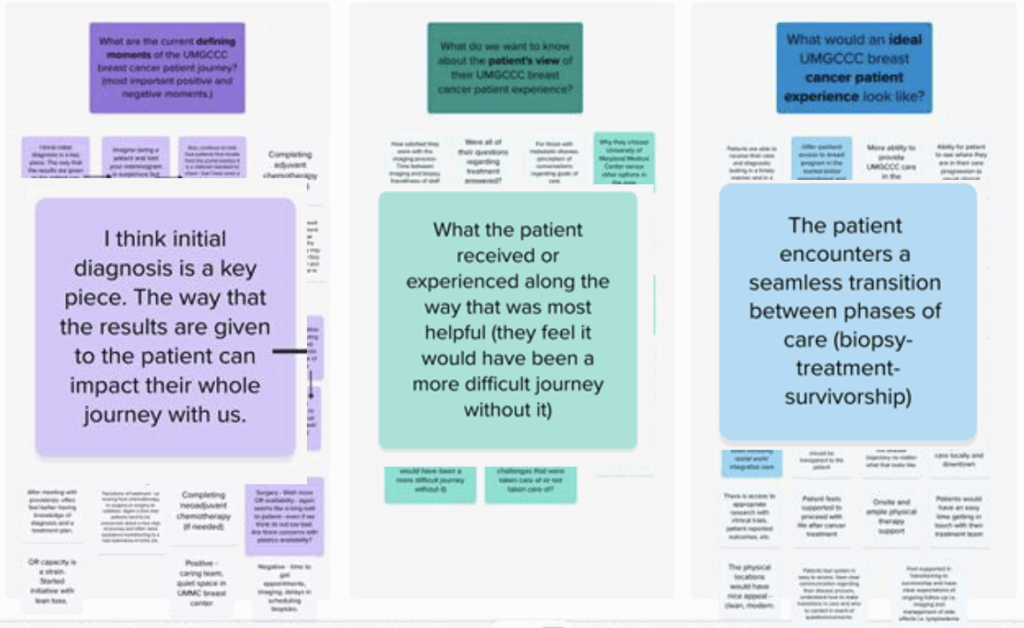
During the workshop, attendees responded to questions about the patient journey: What are the current defining moments of the UMGCCC breast cancer patient journey (most important positive and negative moments? What do we want to know about the patient’s view of their UMGCCC breast cancer patient experience? What would an ideal UMGCCC breast cancer patient experience look like?
“This phase is absolutely critical,” says McMahon. “You’re getting stakeholder alignment from go and keeping them connected to the project as it advances. Then when you have the insights, you’ll have the buy-in and support to actualize changes to better serve patients.”
Step 3: Patient Journey Mapping
Understanding the moments that matter.
Cast & Hue talked to 19 patients (14 from UMGCCC and five from other Baltimore cancer centers) who had completed core treatments in the past year.
“In journey mapping, it’s important to think about when the experience happened,” explains Koch. “Cancer is a significant life event people remember, so we felt comfortable going back a year. But if we’d been focused on the emergency department, we probably wouldn’t go back more than three months, because those details start to fade.”
“…the real value is breaking down the rigid construct that usually exists between patients and providers and hearing directly from patients.”
Jim McMahon
University of Maryland Medical SystemOne of the big decisions to make in journey mapping is whether conversations will be in-person in a group or virtual and individual.
In-person group workshops are collaborative and can be a deeply empathetic experience. Stakeholders can attend. But there are geographic and timing constraints, as all participants need to be in one place at one time. Travel and location arrangements add expense.
Virtual individual conversations allow for more sensitive discussions. They’re easier for patients with travel limitations, decrease geographic and timing constraints, and are lower cost. Modern tools that allow recording, non-participant observation, and transcription are also an advantage.
“Regardless of virtual or in-person, the real value is breaking down the rigid construct that usually exists between patients and providers and hearing directly from patients,” McMahon says.
UMMS and Cast & Hue chose to conduct conversations virtually, making sure to follow the three most important recommendations for effective patient journey mapping:
- Examine each touchpoint.
- Within each touchpoint, ask what patients were thinking, feeling, and doing.
- Explore the why behind patients’ actions.
Step 4: Final Presentation & Journey Map
Reviewing the findings and making impactful improvements.
Once conversations were complete, Cast & Hue used a spreadsheet and the AI research tool Condens to analyze and code data for types of touchpoints, emotions, defining moments, and themes.
The completed patient journey map started with a summary of self-detection and then mapped out subsequent phases from diagnosis to the end of care. Key insights and patient quotes contextualized the two emotions most identified in the journey mapping: hopeful and worried/nervous. Recurring themes and defining moments from each phase were displayed at the bottom of the map.
“At the end, the patient journey map becomes an artifact that can go on the wall,” Koch says. “It’s a shared piece of qualitative information more powerful and visual than any presentation deck.”
UMGCCC stakeholders received the completed patient journey map and recordings of some of the most powerful patient anecdotes. The group reviewed the findings and began brainstorming a range of solutions that spanned departments.
“This is the step when teams talk about effort vs. impact, test new experiences, and prioritize based on budget and ease of implementation,” explains Koch.
For example, stakeholders learned that some patients had received suspicious screening results on a Friday afternoon and were unable to get more information from a provider until the following Monday — a very stressful experience.
“Journey mapping helps systems understand each of the defining moments in the patient experience, so they can start to understand the problems.”
Steve Koch
Cast & HueThe group explored better ways to support patients after a suspicious detection, aligning on the need for immediate follow-up from a Cancer Center contact to discuss next steps. This could be implemented in a few ways. An alert system could activate once results were delivered, so staff could proactively reach out to patients. A dedicated hotline could be created to offer support beyond normal working hours.
The Next Journey
Now that breast cancer stakeholders are in the solutioning phase, UMGCCC and Cast & Hue plan to pursue journey mapping with thoracic and colorectal cancer patients next.
McMahon is eager to eventually see what the three subsets of cancer care patients have in common, and what design thinking solutions can be worked on at scale. Some challenges may transcend departments and specialties. There could be regulatory implications or a need for global IT transformation.
As the breast cancer patient experience evolves based on findings from journey mapping, UMGCCC will assess the impact of changes through HCAHPS scores, patient follow-up, and mystery shopping.
“This could be a proof of concept for the entire organization, if we can demonstrate that the resulting adjustments made a difference to our patients,” says McMahon.
Note: Jim McMahon and Steve Koch presented at the Healthcare Marketing & Physician Strategies Summit on May 2, 2025.
Amanda Green is an award-winning creative director and writer who helps brands and organizations share their stories through custom articles, video, social, audio, and events that spark curiosity, stir emotions, and inspire action. Reach her on LinkedIn.
Related Articles
Keys to Effective Health System Service Line Planning for the Future
